AFK Weekly newsletter 3
In just 30 minutes, you will get some really important concepts for AFK.
-
Explain the answers in details.
-
Quick recap for the whole concept.
#Operative
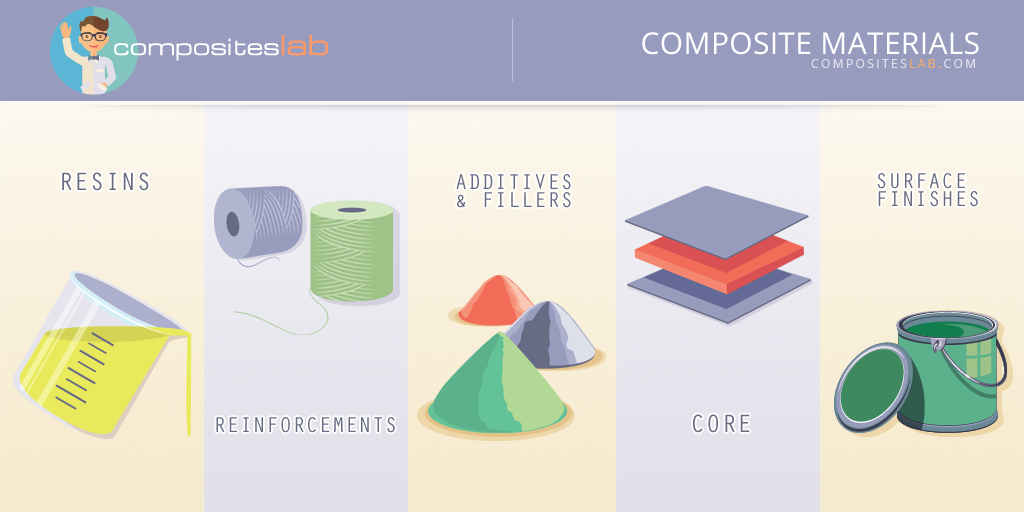
1-increasing the volume of fillers in composite resin
will cause all of the following, except:
◯ a. increased hardness or strength
◯ b. Increase polymerization shrinkage
◯ c. lower thermal expansion coefficient
◯ d. increase of compression strength
1-increasing the volume of fillers in composite resin will cause all of the following, except:
◯ a. increased hardness or strength
◯ b. Increase polymerization shrinkage
◯ c. lower thermal expansion coefficient
◯ d. increase of compression strength
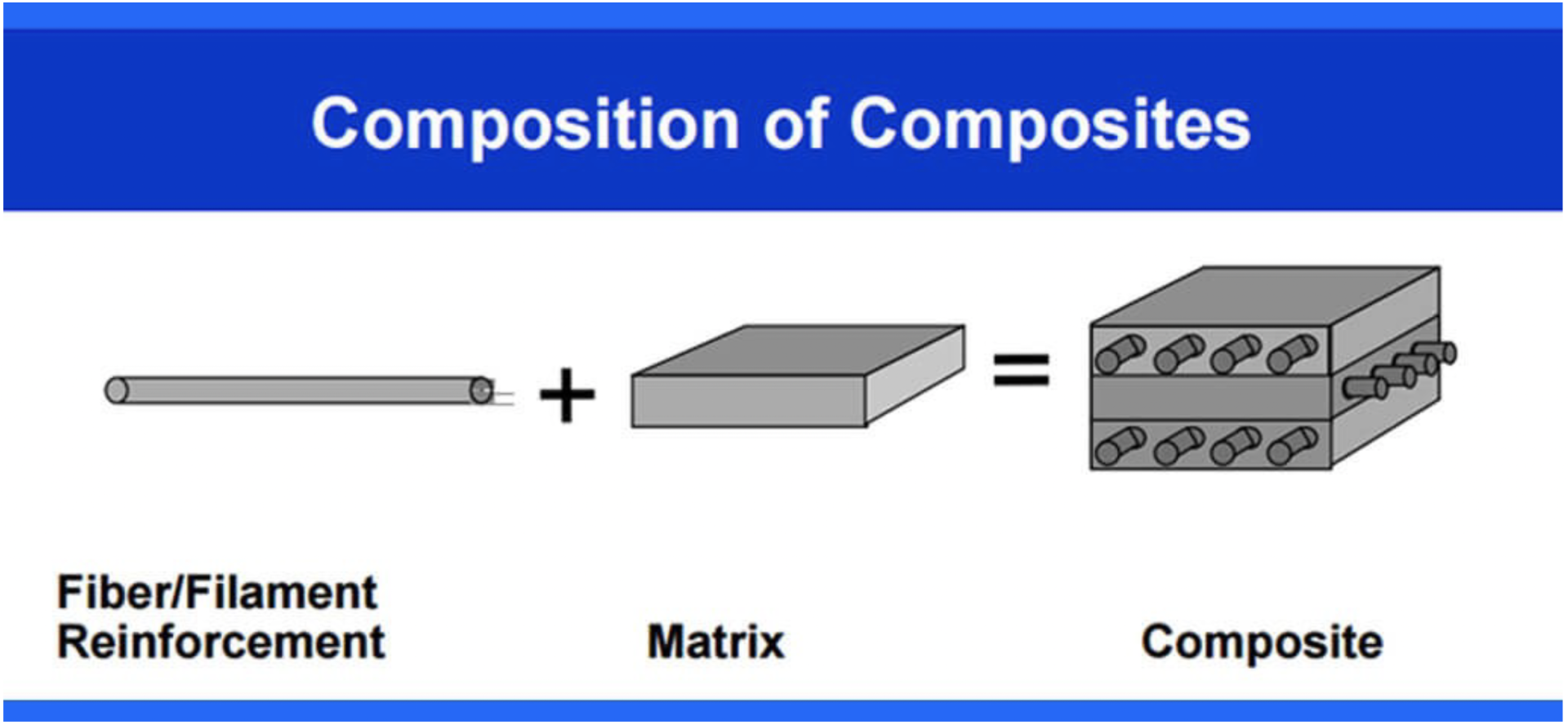
- Function of the fillers in the composite are:
#Pharma
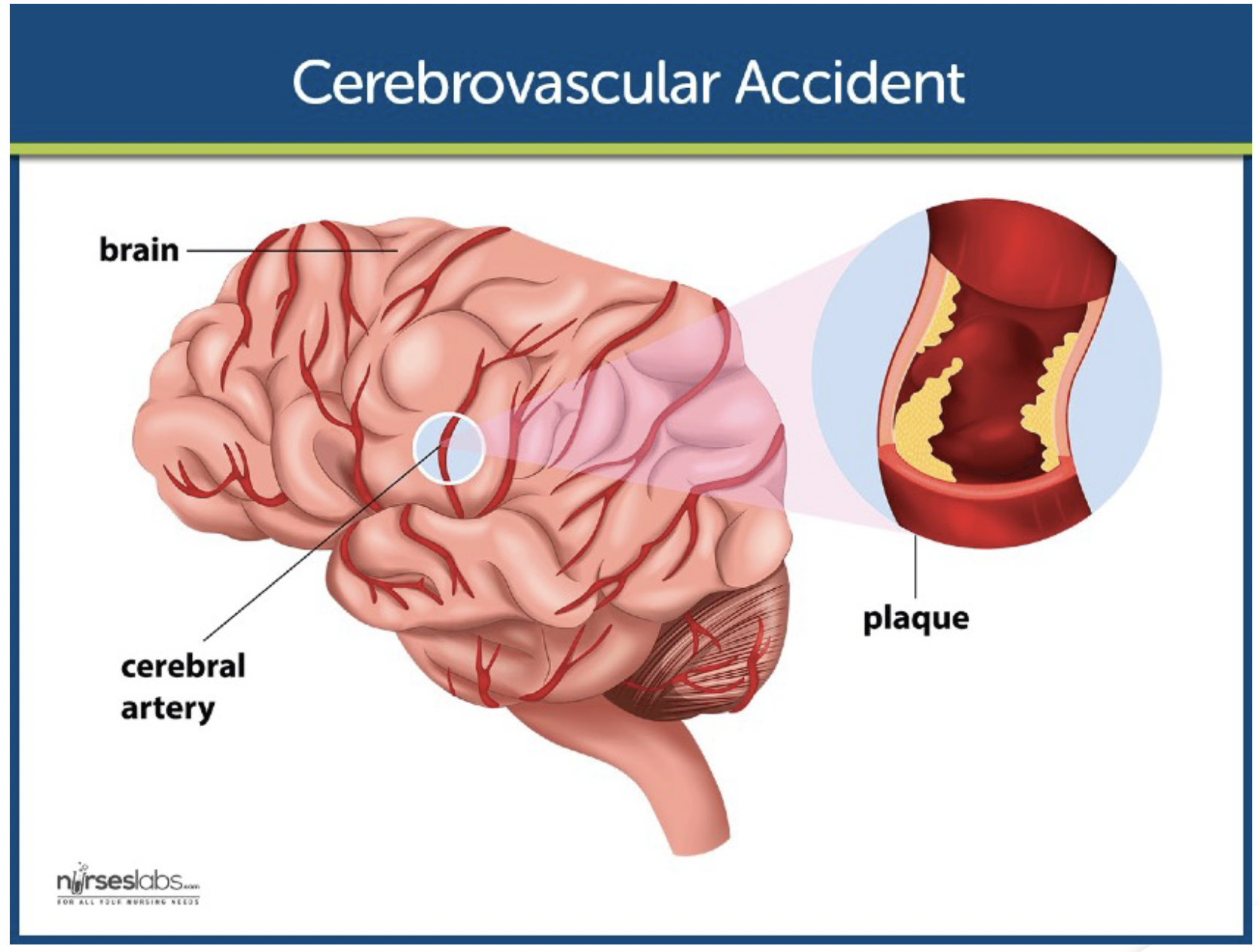
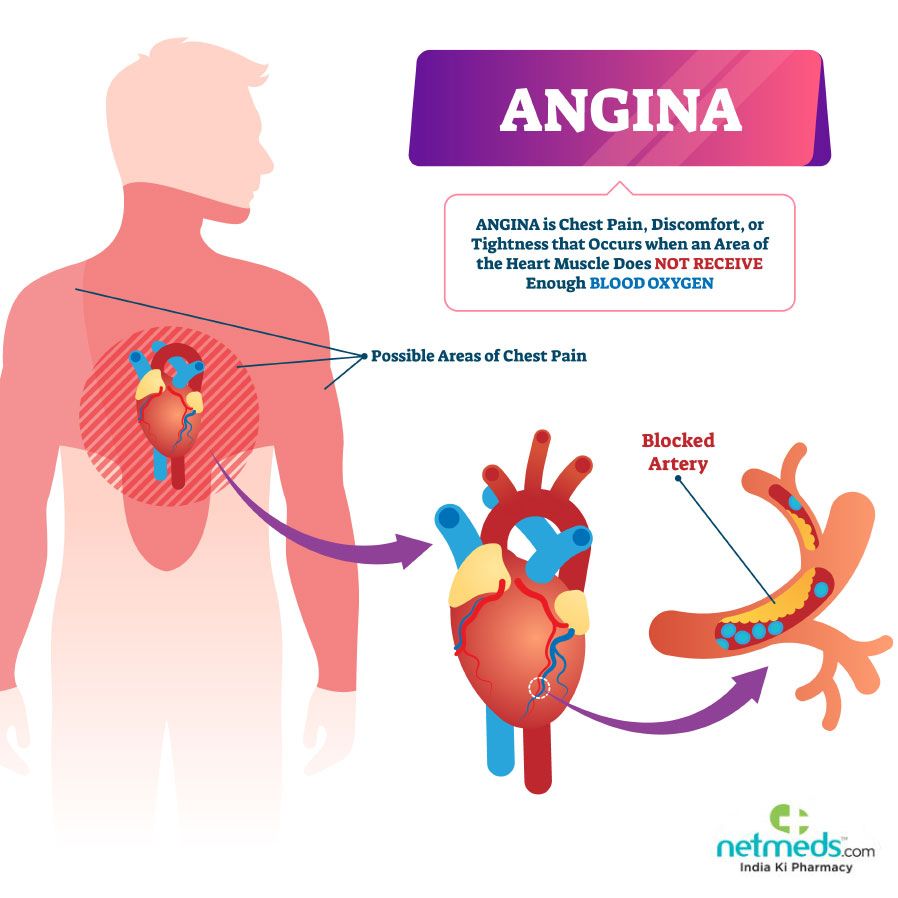
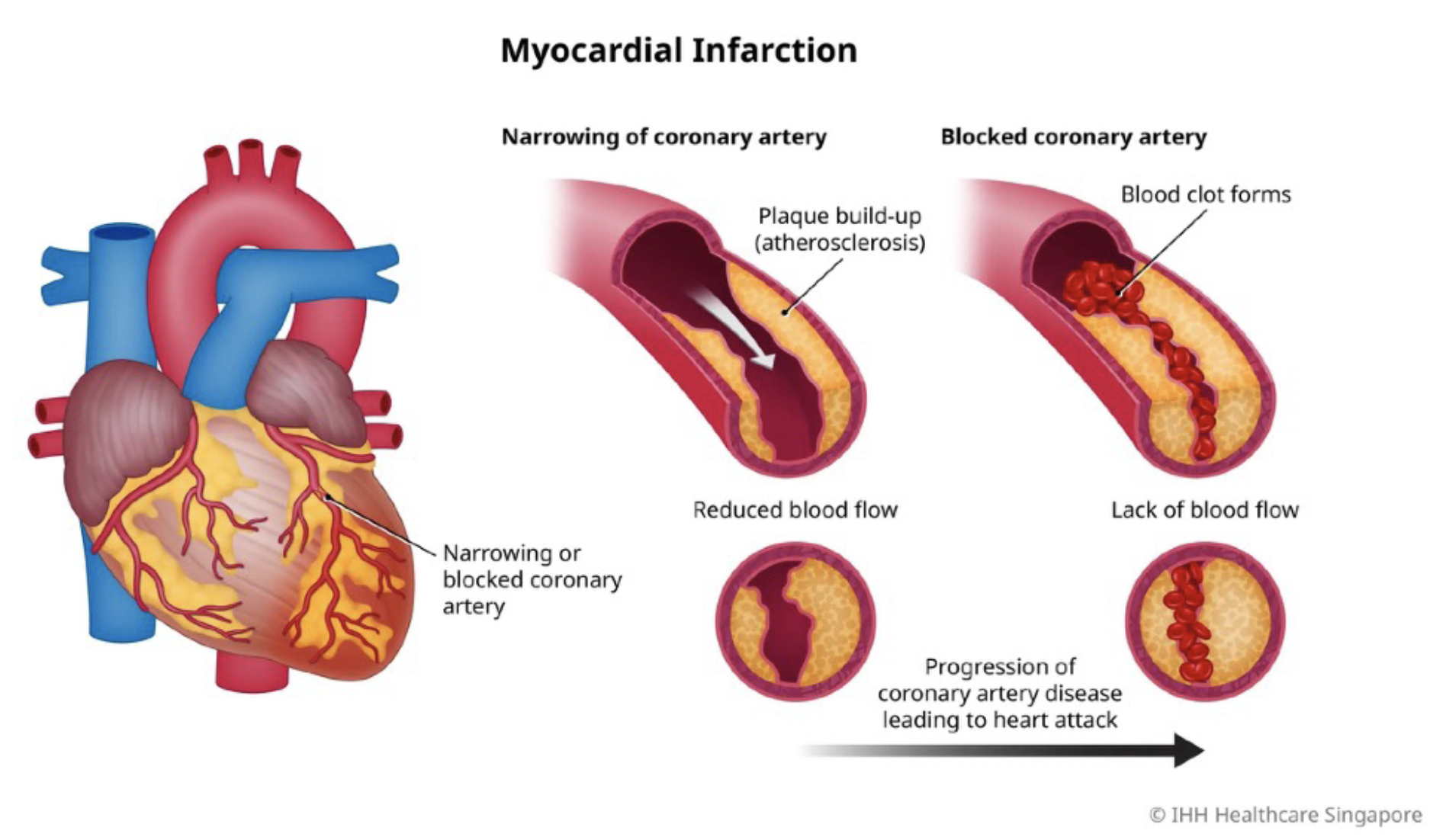
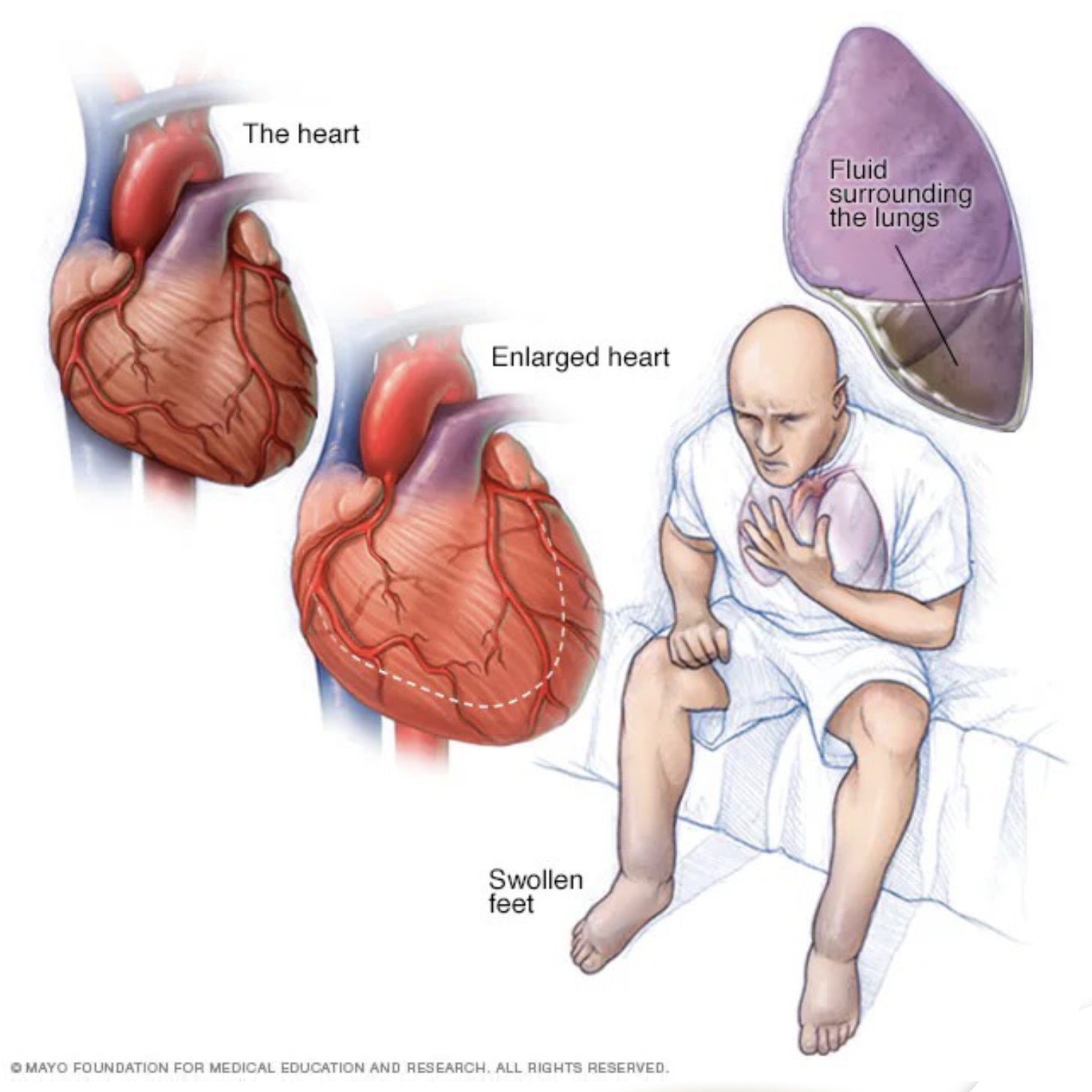
2-A patient is taking Atenolol, Ososorbide Mononitrate
and Diltiazem (Cardiazem). The most likely diagnosis
is:
◯ A. Atrial fibrillation and congestive heart failure
◯ B. Congestive heart failure and myocardial infarction
◯ C. Cardiac ischemic disease and hypertension
◯ D. Myocardial infarction and ventricular arrhythmia
2-A patient is taking Atenolol, Ososorbide Mononitrate and Diltiazem (Cardiazem). The most likely diagnosis is:
◯ A. Atrial fibrillation and congestive heart failure
◯ B. Congestive heart failure and myocardial infarction
◯ C. Cardiac ischemic disease and hypertension
◯ D. Myocardial infarction and ventricular arrhythmia
Join our AFK Weekly newsletter
Solving questions is really important, but solving exam grade questions with true and authenticated answers is critical.
Will post a question everyday, then at the week end will do a video to explain the correct answers and the concept of each questions, signup now to get weekly updates.
Will post a question everyday, then at the week end will do a video to explain the correct answers and the concept of each questions, signup now to get weekly updates.
Thank you!
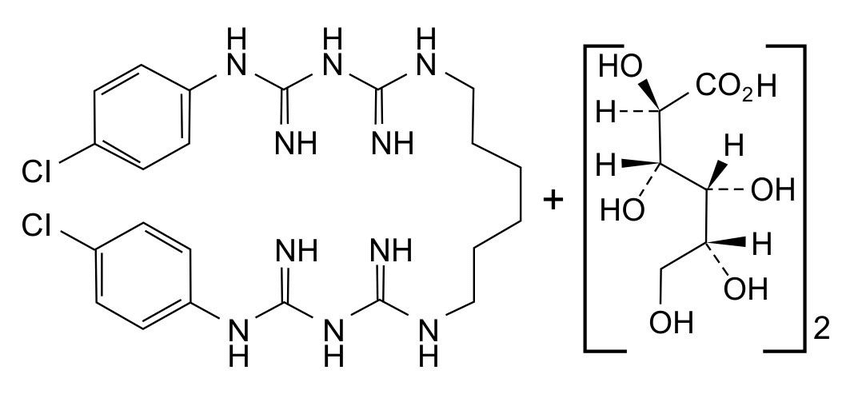
#Periodontology 3- Chlorhexidine mouth rinses act on:◯ A. Streptococcus mutans
◯ B. Lactobacilli
◯ C. streptococcus pyogenes
◯ D. Candida albicans
◯ A. Streptococcus mutans
◯ B. Lactobacilli
◯ C. streptococcus pyogenes
◯ D. Candida albicans
◯ B. Lactobacilli
◯ C. streptococcus pyogenes
◯ D. Candida albicans
-Chlorhexidine (CHX) is effective against a wide range of bacteria, including both gram-positive and gram-negative species. Some of the bacteria that Chlorhexidine is particularly effective against include:
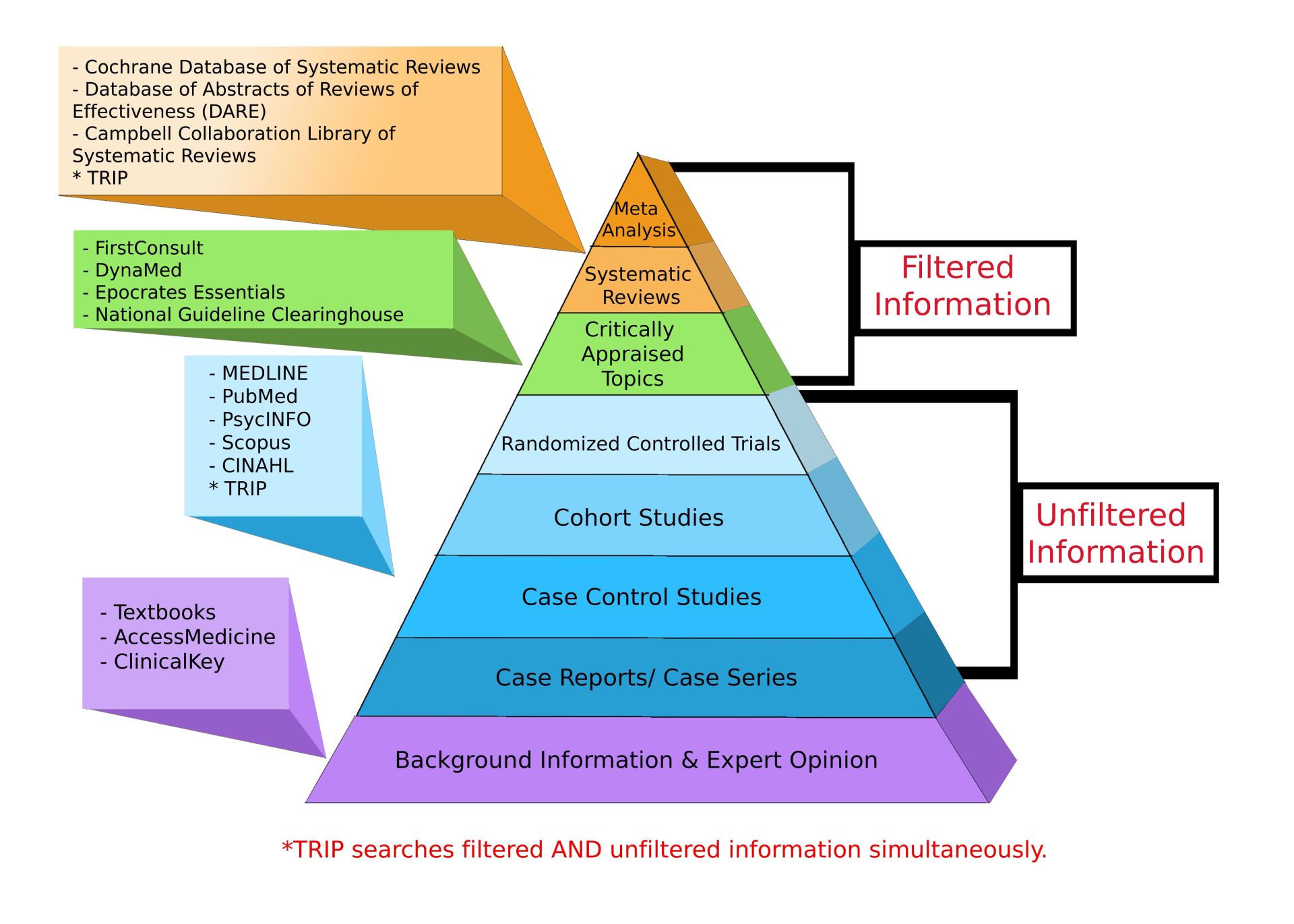
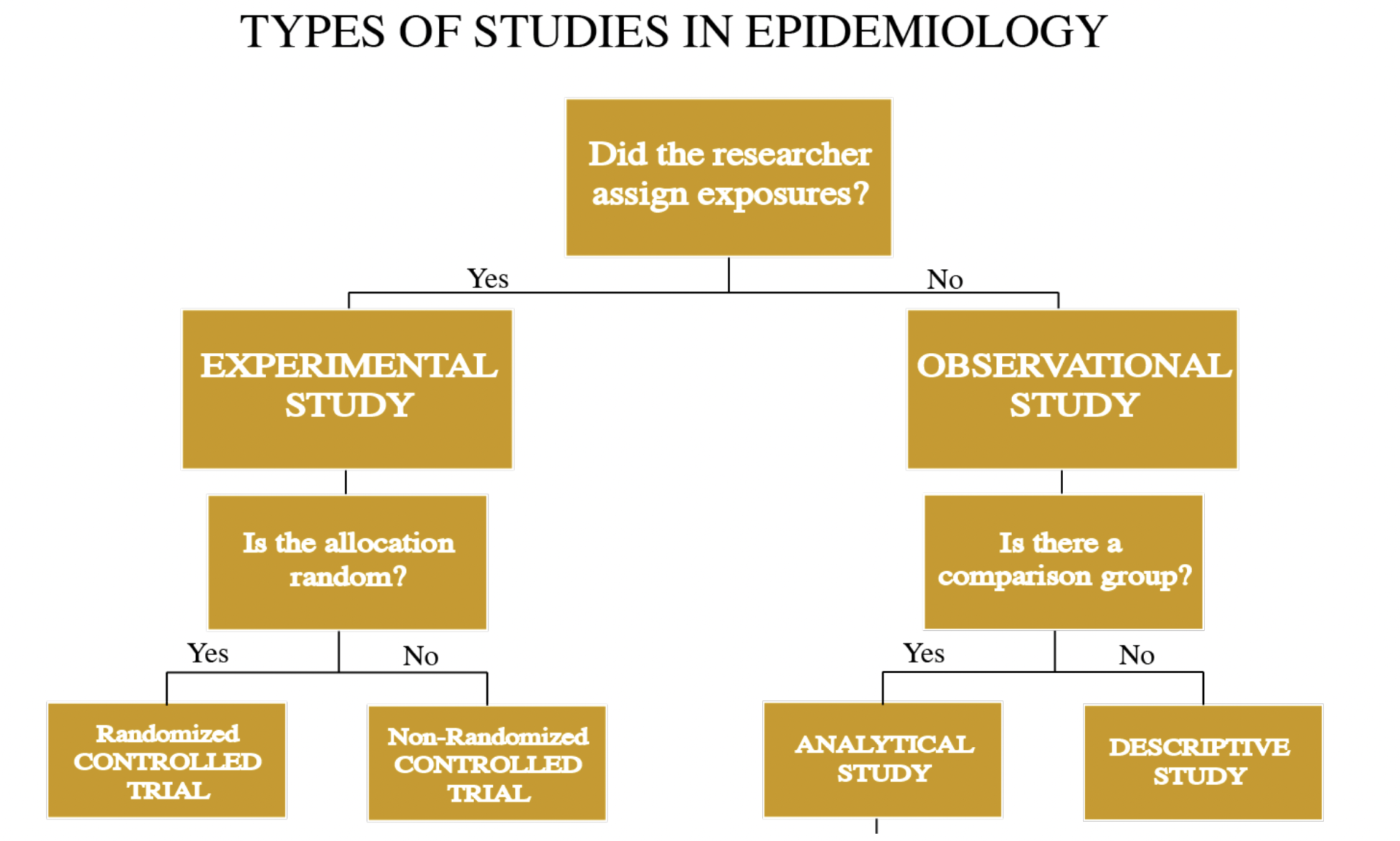
#Epidmology
4-Which of the following provides the best information
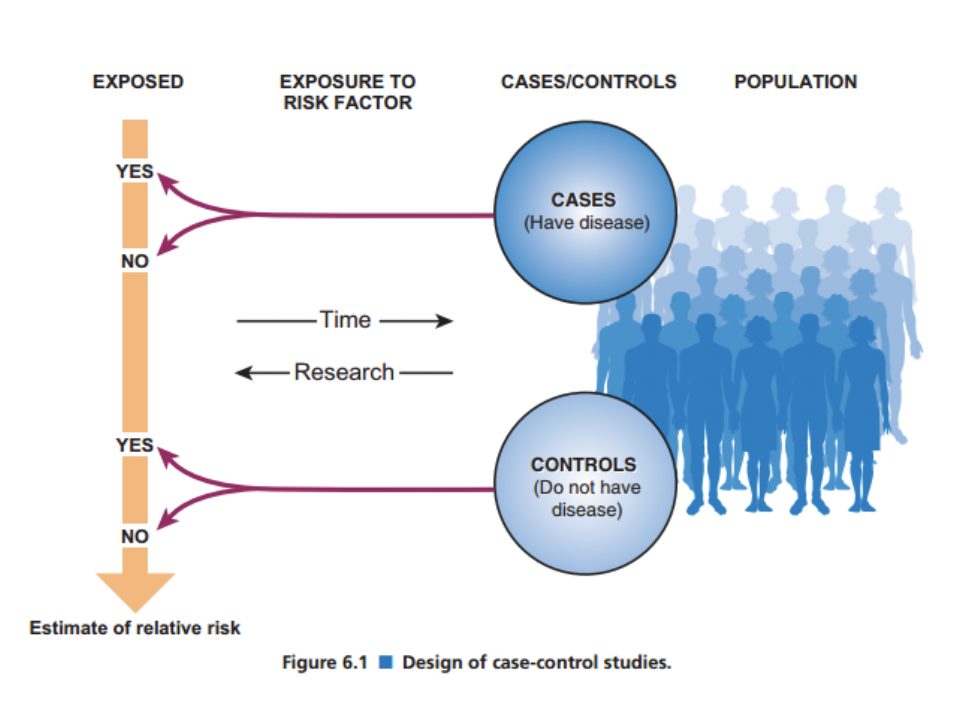
according to evidence based dentistry?◯ A. Case-Control studies
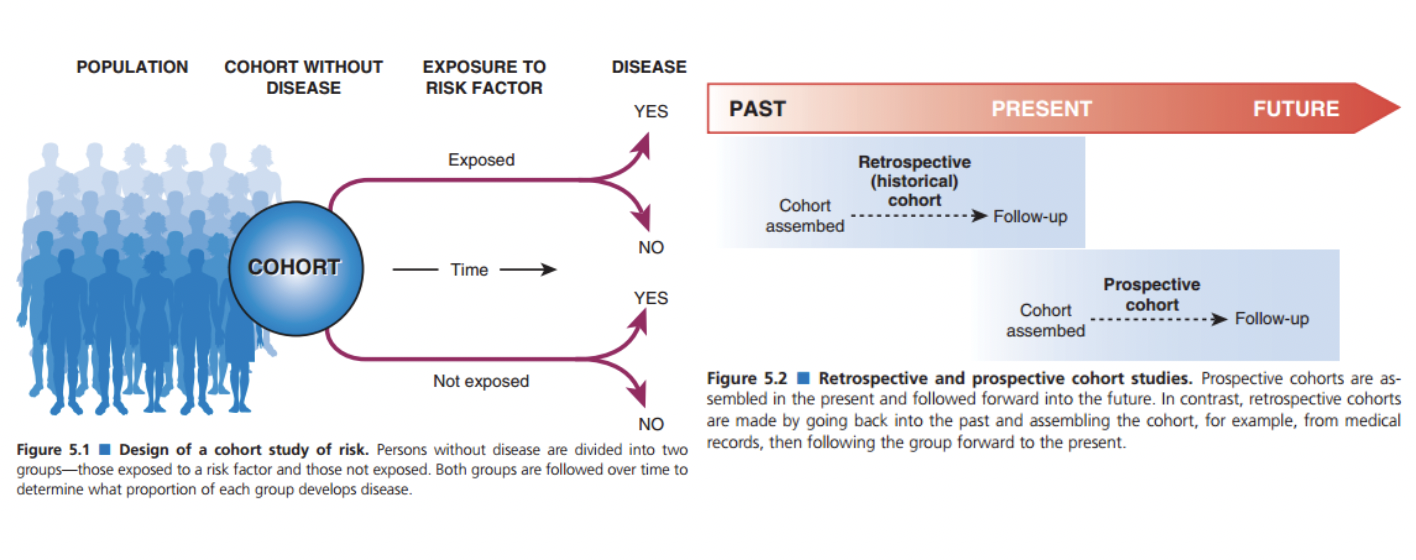
◯ B. Cohort studies
◯ C. Randomized clinical trails
◯ D. Systematic reviews
4-Which of the following provides the best information according to evidence based dentistry?
◯ B. Cohort studies
◯ C. Randomized clinical trails
◯ D. Systematic reviews

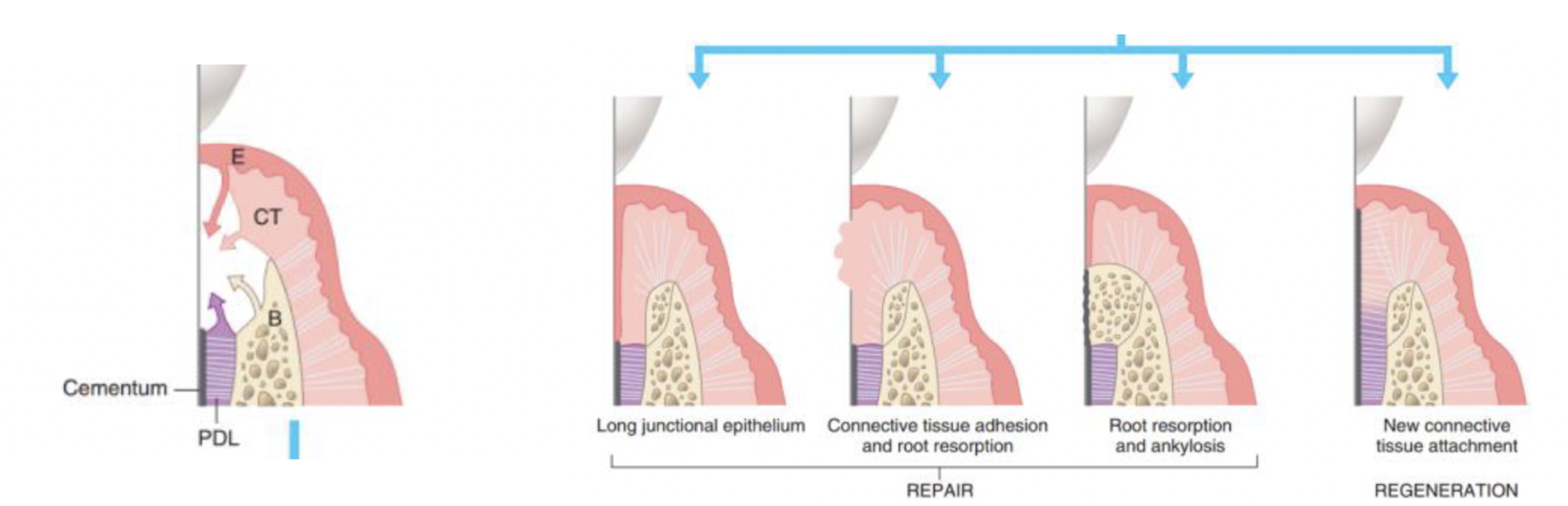
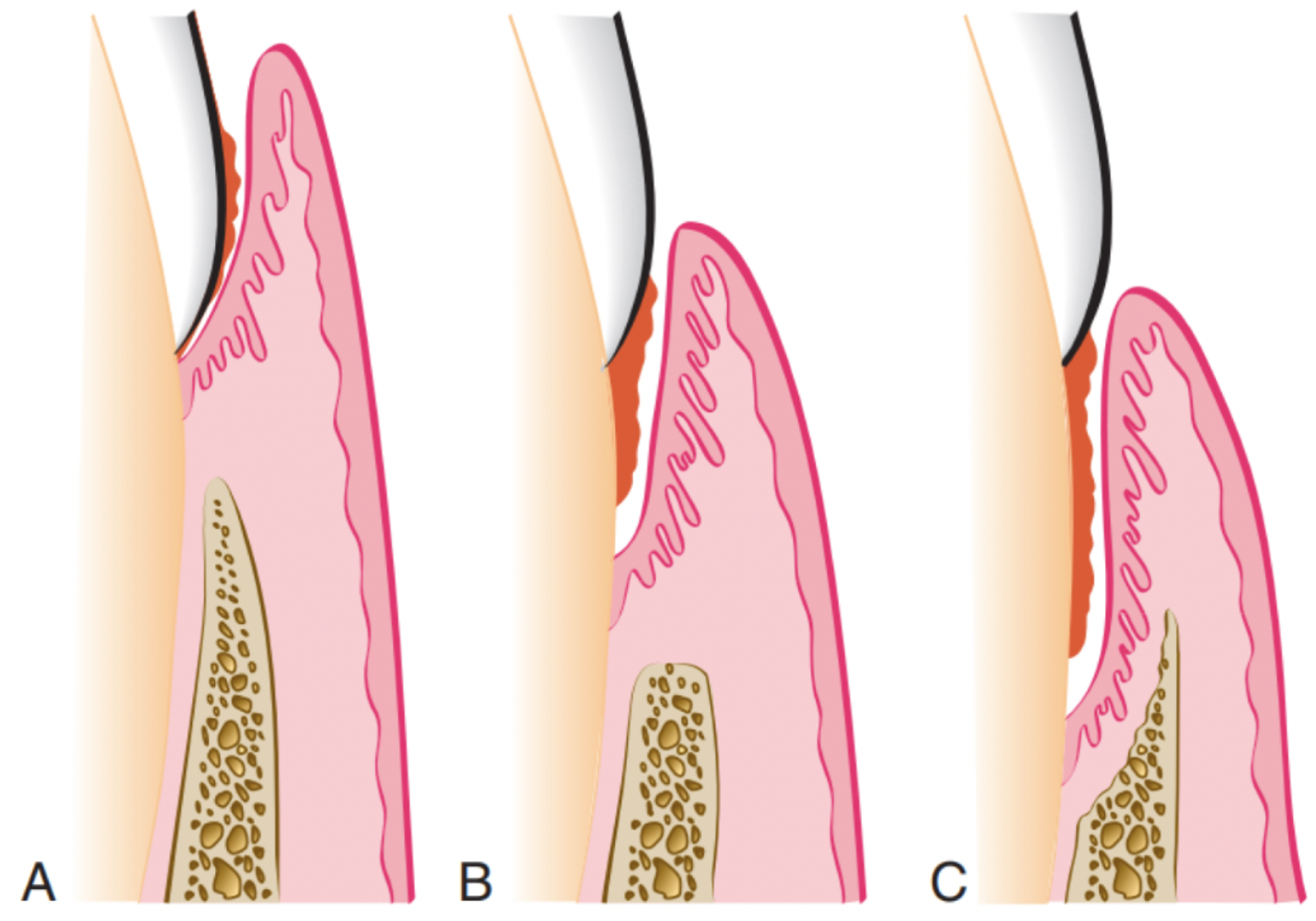
#Periodontology 5-A patient has a pocket depth of 6mm and attachment
loss of 5.5 mm, what is the correct treatment in this
case?
◯A. Scaling and root canal
◯ B. Oral hygiene measures
◯ C. Comprehensive treatment
◯ D. Surgical intervention
◯A. Scaling and root canal
◯ B. Oral hygiene measures
◯ C. Comprehensive treatment
◯ D. Surgical intervention